Causes of the development of basal cell carcinoma
Basal cell carcinoma (basal cell cancer or basalioma) accounts for 75 % of all cases. Basal cell carcinoma used to occur more frequently in women and men over 60 years of age, but recently younger people have also been affected by white skin cancer. Basal cell carcinoma develops from the cells of the so-called basal cell layer of the skin and mainly occurs in the head or neck area. The nose, lips, neck or forehead are particularly at risk.
The exact cause is not yet fully understood. However, an important factor in the development of basal cell carcinoma is UV radiation, especially when it hits unprotected skin. It does not matter whether it is artificial (solarium) or natural (sunbathing) UV radiation. A adequate sun protection with a high sun protection factor is therefore Prevention of skin cancer indispensable. People with light skin types and older people with poorer immune systems have a higher risk of developing basal cell carcinoma.
If one notices signs on sun-exposed skin, it is usually already a cancerous tumour that must be removed. In the vast majority of cases, however, there is a complete chance of recovery with competent treatment.
How do I recognise basal cell carcinoma?
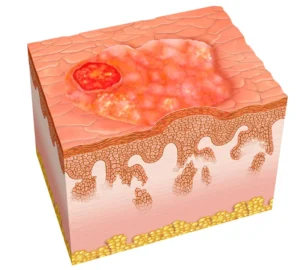
This type of skin cancer is very diverse. Mostly wax-coloured nodes or patches form at the beginning, later skin-coloured to reddish. Basal cell carcinoma can also look like a shiny bump or scar and sometimes bleed.
The squamous cell carcinoma
Harmless skin changes, the actinic keratoses (fine scales on the surface of the skin) develop into solid spots that can initially be scraped off, but subsequently become keratinised and firmly adhere. In the centre of these spots, a lump later forms that grows rapidly.

Diagnosis:
It is important at the first sign to seek competent advice. Dermatologist or a Dermatologist to visit. Dermatoscopy (reflected-light microscopy) is used to look at the skin with a microscope down to the deeper layers. Skin changes can be clearly magnified so that it is usually possible to determine immediately whether it is a benign change in the skin or a form of cancer. In unclear cases, a biopsy (taking a sample) can provide certainty.
In our surgeries in Vienna and Tulln, you will find empathetic and competent advice as well as a wide range of state-of-the-art therapies.
Treatment options for white skin cancer
Operation:
The standard treatment for white skin cancer is surgery. The tumour is removed completely into the healthy tissue. The operation is performed under local anaesthesia.
Cryotherapy
The form of therapy with liquid nitrogen (-196 °C) is used to destroy cancer cells in small superficial forms of white skin cancer and actinic keratoses (early stages of squamous cell carcinoma).
Photodynamic therapy (PDT)
Photodynamic therapy (PDT) is a modern, gentle procedure that uses photochemical processes to treat tumours and skin diseases and is a good alternative to surgical removal. In contrast to conventional methods, the dermatologist achieves better cosmetic results with PDT (no scarring).
PDT treatment procedure
First, the most severely affected areas are treated with the Laser pre-treated.
Afterwards, a special cream, the so-called photosensitizer, is applied to the skin for three hours, which accumulates especially in the skin cancer cells (topical application).
After their exposure time, the skin is exposed to visible, intense light of a certain wavelength, which leads to the formation of oxygen radicals and the destruction of pathologically changed cells. A distinction is made between primary cytotoxicity, which primarily damages the cells, and secondary cytotoxicity of the photosensitizer, which affects the blood vessels (systemic effect).
Photodynamic therapy has proven itself well in the treatment of actinic keratoses and basaliomas. The actual treatment takes only 10 to 20 minutes and can be repeated at intervals of two weeks. To avoid pain during or after the therapy, either painkilling medication or gels are administered.
Healthy tissue is largely spared during photodynamic therapy. After the treatment, inflammation of the affected skin area occurs for a few days, which confirms the effectiveness of the therapy and is harmless.
Local therapy with imiquimod ointment:
Imiquimod stimulates the immune response to tumour cells by promoting the production of immune system messenger substances called cytokines (for large superficial basal cell carcinomas). Inflammatory reactions, burning and pain may occur.
Prevent white skin cancer
Vitamins and antioxidants: Nicotinamide (vitamin B3) in high doses is said to stimulate the mechanism for self-repair of DNA and counteract UV damage in cells.
The aggressiveness of cancer cells of the skin can be reduced with the help of vitamin D.
(Have vitamin D levels checked in the laboratory).
Raspberries, blackberries and strawberries contain large amounts of ellagic acid, which is able to render all carcinogenic substances in the body harmless.
Skin cancer screening: It is best to avoid excessive sun exposure. If in the sun, then only with high sun protection!